Do you know your Apo-B levels? If you don’t, you should.
When your Apo-B is high, so is your risk of dying from a heart attack and cardiovascular disease. The good news is you can lower it through lifestyle and personalized interventions.
In this edition is all about ApoB. You chose how far do you want to go: flyover with a clear summary, a ground work with a patient case and clinical insights, and a deep dive for my fellow nerds. Grab a cup a tea or coffee and let me tell you why you should get to know your ApoB. Oh, and if you are wondering what is ApoB, it is a backbone of every lipid particle including your “bad cholesterol”.
Don’t Settle. Look Beyond Borderline.
She was a medical professional in her 40s who loved to hike and stay active. A few years earlier, she developed gestational diabetes that “resolved” after pregnancy. Her A1c returned to 5.8, back in the prediabetic range. Her doctor wasn’t concerned.
She asked about using a continuous glucose monitor. “You don’t need it,” she was told. Insurance wouldn’t cover it since she wasn’t diabetic, and tracking glucose might only cause anxiety.
So, she continued with her annual labs. The results were normal or borderline, including cholesterol. “A little high, but not too bad,” she heard. “Eat better, exercise more.”
When she asked about ApoB, same answer - not necessary. Everything looked acceptable. Except it wasn’t.
You see, her her labs stayed borderline, but trended up: LDL rose from 100 to 130 to 145 mg/dL and A1c hovered between 5.6 and 6.0 percent.
Nothing super urgent. When numbers rose, she ate better and trained harder. Labs improved. On paper, things looked controlled. Until things started to change.
Unknowingly, she was in perimenopause. Relentless waves of middle-of-the-night awakenings and sweats. She could not recall what she had for breakfast the day before, and she had no energy despite loading up on carbs.
She continued to treat her labs like a test she could cram for. I’ll fix it next time, just give me 3 months. Yet, nothing was being fixed. While LDL and A1c hovered near “normal,” atherogenic particles, were insidiously circulating through her body.
She was trapped in the borderline of standard tests. Not once was her Apo-B checked.
Why it matters, you ask?
Here is the most important one liner of this entire masterclass newsletter:
ApoB counts the cholesterol-carrying particles that actually drive atherosclerosis and heart disease.
PART I. Flyover (tldr)
You have to look beyond standard test and borderline results. Here is why:
THE PROBLEM
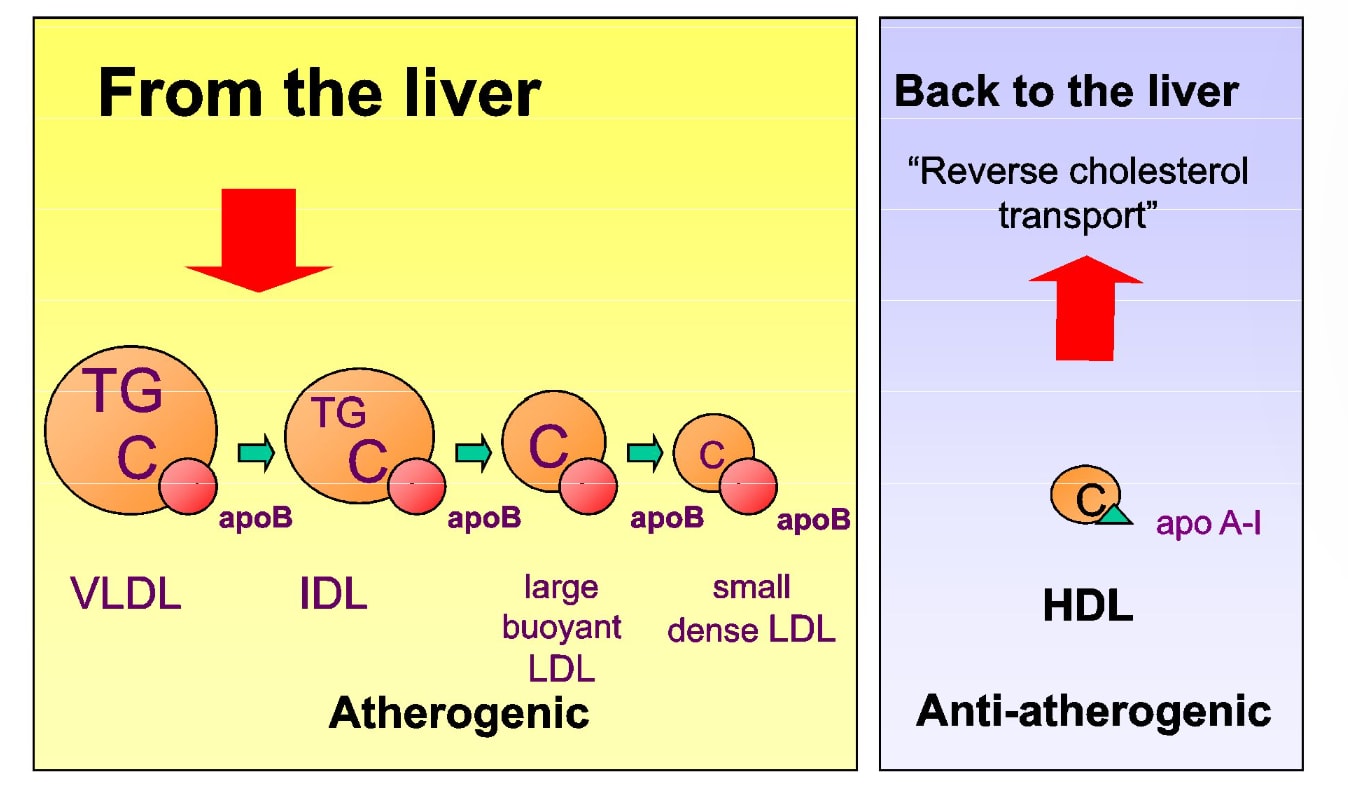
Most clinicians still use standard testing of LDL cholesterol (LDL-C) to assess heart disease risk. This is not enough. LDL-C measures how much cholesterol is inside particles, not how many particles are actually damaging the arteries - which is what Apo-B will tell you.
WHY THIS MATTERS TO YOU
You can have “normal” LDL-C and still carry too many atherogenic particles. This mismatch is common in people with insulin resistance, metabolic syndrome, and fatty liver, the core drivers of cardiometabolic disease, including heart attacks.
WHAT CURRENT PRACTICE MISSES
ApoB (apolipoprotein B) is the protein found on every atherogenic particle. Because of this, ApoB is a direct particle count and predicts cardiovascular events more accurately than LDL-C, especially when the two don’t agree.
What you’ll learn in this edition
How ApoB particles drive plaque at the arterial wall
Why particle number (ApoB) matters more than LDL-C
How insulin resistance and fatty liver push ApoB up
A practical framework to test, interpret, and lower ApoB
A case where conventional testing said “you’re fine” while biology said otherwise
Deep dive into multiomics testing and guided framework
YOUR MAIN TAKEAWAY
If you have insulin resistance, metabolic syndrome, prediabetes/diabetes, fatty liver, are peri/menopausal, or have a family history of early heart disease, you are at risk AND checking your ApoB is NOT optional. LDL-C alone is not going to tell you what you really need to know.
Numbers to remember:
Longevity/prevention: <70–80 mg/dL
High risk (ASCVD, diabetes, strong family history): <65–70 mg/dL
(Do you know your ApoB numbers? Leave a comment below and share what you have learn from them)
PART II: Ground Work
The Patient Who Chose a Different Gift for Herself Last Christmas
Last December, this patient did something she has not done before. She got tired of feeling tired while helping others feel better.
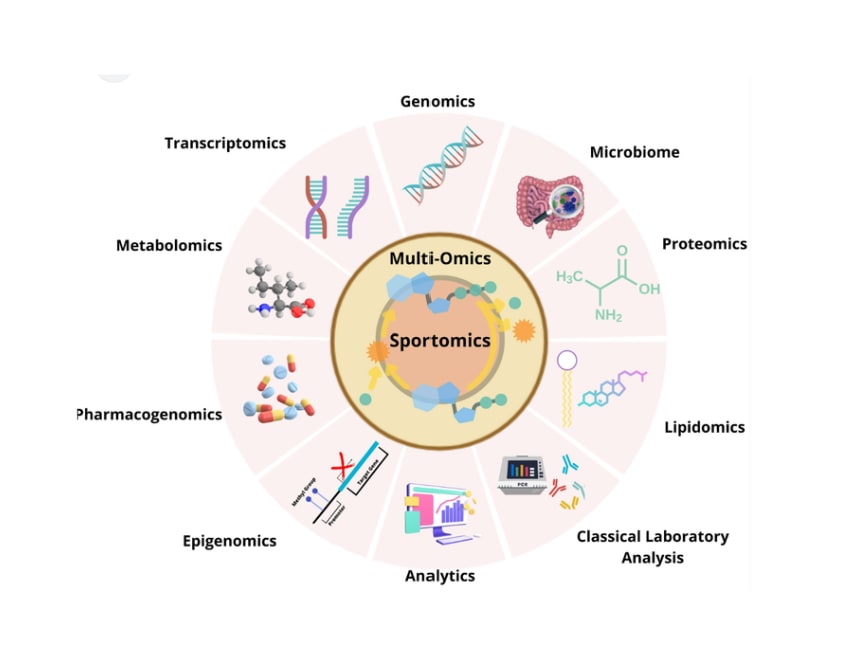
Instead of buying herself another bag, she treated herself with a “Christmas gift to protect my future”. The most comprehensive dive into her biology through advanced cardiometabolic and multiomics testing (more on this in deep dive section).
These are not your typical annual labs. Most are not covered by insurance. Most clinicians are not trained to interpret them. These are advanced clinical tests she had been recommending and using for her own patients, but kept postponing for herself:
ApoB
Lp(a)
hsCRP and other inflammatory markers
HOMA-IR
And multiomic testing from thousands of other biomarkers from genes, gut, metabolome, mitochondria, etc. Multiomics is a whole different way of understanding human body, health, and disease. It is beyond Medicine 3.0. It is the future of medicine. Here is a quick snapshot of what we can assess with multiomics:
When the results came back, they were not mildly off as she expected. They were a wildy off. Including her clinical biomarkers (which you can get from your doctor, if you know what to ask for):
A1c: 8.3%
No longer “borderline.” Full-blown type 2 diabetes!
ApoB: 127 mg/dL
Atherogenic particle burden in a high-risk range, especially in the context of diabetes.
ApoB/Apo A1 ratio: 0.72
LDL-C: 154 mg/dL
Borderline high, but not extreme by conventional standards.
LDL particle number 2806 nmol/L
Optimal: < 1,000
LDL pattern: B
Small, dense LDL particles (higher risk)
Total cholesterol: 235 mg/dL
Borderline high
Fibrinogen antigen: 352 mg/dL
hsCRP: 1.9 mg/L
Low-grade chronic inflammation.
Elevated liver enzymes
Vitamin D: 25 ng/mL and below range despite supplementation.
This is what a metabolic storm looks like. If not corrected, it shortens your healthspan (years lived in good health) and lifespan (years lived).
If you are thinking, what do all these results have to do with ApoB, great question! ApoB is the final common pathway. Insulin resistance, fatty liver, inflammation, and hormonal shifts in perimenopause all push the liver to produce more cholesterol-carrying particles AND slow their clearance. Each of those particles carries one ApoB. That’s how risk accumulates even when LDL-C and routine labs look acceptable.
What caused it?
Years of chronic stress, poor sleep, and carb-driven exhaustion overwhelmed her metabolic capacity. Excess fuel spilled into the liver, where it was converted to fat and exported as ApoB-containing particles into the bloodstream.
Hormonal shifts, including estrogen decline, chronic cortisol elevation, and low thyroid activity, reduce LDL receptor function and insulin sensitivity, impairing ApoB clearance and increasing atherogenic particle burden.
Genetics set the backdrop: a predisposition to fatty liver, diabetes, and cardiovascular disease. Perimenopause accelerated the process as insulin sensitivity declined.
You’ve heard it before: “Genes load the gun, lifestyle pulls the trigger.”
It’s true. And for her, the trigger had been pulled, but we caught it in time.
Genes are not destiny, but they establish boundaries.
Lifestyle determines whether those boundaries are crossed.
Her physiology had been drifting in this direction for years. The deep dive and personalized roadmap empowered her to change the course so she can live healthy for long. Break her family course.